Researchers at the Massachusetts Institute of Technology, Brigham and Women’s Hospital, and Harvard Medical School have developed a potential new treatment for alopecia areata. Alopecia areata is an autoimmune disease that causes hair loss and affects people of all ages, including children.
Most patients with this type of hair loss have no effective treatment. Researchers have developed a microneedle patch that can be applied painlessly to the scalp and stops autoimmune attacks by releasing drugs that help rebalance the immune response in the area.
In a study in mice, researchers found that the treatment caused hair to regrow and dramatically reduced inflammation in the treated area, while avoiding systemic immune effects in other parts of the body. . The researchers say this strategy could also be applied to treat other autoimmune skin diseases such as vitiligo, atopic dermatitis, and psoriasis.
“This innovative approach represents a paradigm shift. Rather than suppressing the immune system, we now focus on precisely controlling the immune system at the site of antigen encounter to create immune tolerance. ,” says Natalie Artzi, principal investigator and associate professor of medicine at MIT’s Institute of Biomedical Engineering and Science. He received his doctorate from Harvard Medical School and Brigham and Women’s Hospital and is an associate faculty member at Harvard’s Wyss Institute.
Artzi and Jamil R. Azzi, an associate professor of medicine at Harvard Medical School and Brigham and Women’s Hospital, are senior authors of the new study, which is published in the journal Advanced Materials. Nour Younis, a postdoctoral fellow at Brigham and Women’s, and Nuria Puigmal, a postdoctoral fellow at Brigham and Women’s and formerly of MIT Research, are the paper’s lead authors.
The researchers are now working on starting a company to further develop the technology, led by Puigmal, who was recently awarded a Harvard Business School Blavatnik Fellowship.
Direct delivery
Alopecia areata, which affects more than 6 million Americans, occurs when the body’s own T cells attack the hair follicles, causing hair to fall out. Scalp injections of immunosuppressive steroids, the only treatment available to most patients, are painful and often cannot be tolerated by patients.
Some patients with alopecia areata and other autoimmune skin diseases can also be treated with oral immunosuppressive drugs, but these drugs lead to widespread suppression of the immune system and Harmful side effects may occur.
“This approach silences the entire immune system and reduces inflammatory symptoms, but leads to frequent flare-ups. It also increases susceptibility to infections, cardiovascular disease, and cancer,” says Artzi. .
A few years ago, at a working group meeting in Washington, Artzi happened to be sitting next to Azzi, an immunologist and transplant doctor. He was looking for new ways to deliver drugs directly to the skin for skin-related treatments. disease.
Their conversation led to a new collaboration, and the two labs joined forces to develop microneedle patches that deliver drugs to the skin. In 2021, they reported that such patches could be used to prevent rejection after skin grafts. New research has begun to apply this approach to autoimmune skin diseases.
“The skin is the only organ in our bodies that we can see and touch, but when it comes to drug delivery to the skin, we go back to systemic administration. We are using microneedles to locally reprogram the immune system. “We saw great potential in using patches,” says Azzi.
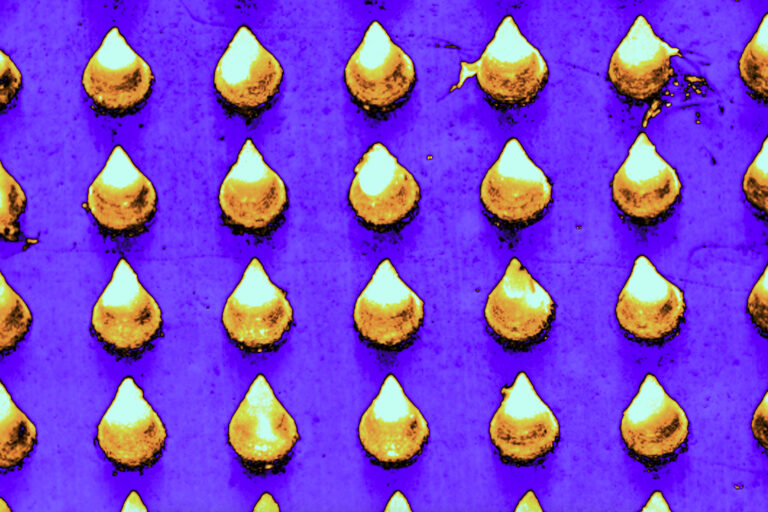
The microneedle patches used in this study were made from hyaluronic acid cross-linked with polyethylene glycol (PEG), both of which are biocompatible and commonly used in medical applications. This delivery method allows the drug to pass through the hard outer layer of the epidermis, which creams applied to the skin cannot penetrate.
“This polymer formulation allows us to create highly durable needles that can effectively penetrate the skin. Additionally, this gives us the flexibility to incorporate any drug,” Artzi said. I say. For this study, the researchers loaded the patch with a combination of the cytokines IL-2 and CCL-22. Together, these immune molecules help recruit regulatory T cells, which proliferate and reduce inflammation. These cells also help the immune system recognize that the hair follicle is not a foreign antigen and stop attacking the hair follicle.
hair regrowth
The researchers found that mice given the patch every other day for three weeks had less inflammation and more regulatory T cells in the area. Hair was able to regrow in those areas, and this growth was maintained for several weeks after treatment ended. In these mice, there were no changes in the levels of regulatory T cells in the spleen or lymph nodes, suggesting that the treatment affected only the patched area.
In another series of experiments, researchers transplanted human skin into mice with humanized immune systems. In these mice, microneedle treatment also induced regulatory T cell proliferation and reduced inflammation.
The researchers designed the microneedle patch so that after releasing the drug payload, it could collect a sample that could be used to monitor the progress of the treatment. When hyaluronic acid enters the skin, it expands the needle approximately 10 times, allowing it to absorb interstitial fluid containing biomolecules and immune cells from the skin.
After patch removal, researchers can analyze the sample to measure levels of regulatory T cells and inflammatory markers. This may prove useful in monitoring future patients who may receive this treatment.
The researchers now plan to further develop this approach for treating alopecia and extend it to other autoimmune skin diseases.
This research was funded by Ignite Fund and Shark Tank Fund awards from the Brigham and Women’s Hospital School of Medicine.